Medical care presents multiple complexities which need creative methods for successful navigation. Through its diverse offering Zelis provides solutions which optimize business operations at reduced expense while enhancing the satisfaction levels of all stakeholders. The solutions from Zelis enable healthcare providers and members and payers to work more efficiently while improving transparency throughout their healthcare experience.

Zelis Network Solutions: Enhancing Healthcare for All
Through Zelis Network Solutions the healthcare ecosystem receives connectivity infrastructure to eliminate system gaps. Zelis builds a unified system which unites providers with members and payers to create value for all participants.
How Zelis Helps Healthcare Providers and Members
Zelis deliver products that offer help and support to healthcare service providers to improve on their service delivery to the patients. These solutions include:
- Improved Access to Data: It benefits providers by providing them with greater understanding on how to deliver patient care in order to inform decision-making.
- Efficient Claims Processing: Improved Work flow management is efficient to the providers hence reduce the burden of paperwork.
Increased Transparency: The people involved can conveniently get informations relating to their health care programs which increases the level of trust.
How Zelis Benefits Payers
In terms of payers, Zelis has effective solutions to deliver claims efficiently and get better results. These include:
- Cost Reduction Tools: Payers can learn where the dollars are going and where they are not getting the best value for their money.
- Enhanced Provider Relationships: Implementations which foster payer-provider collaborations as partners.
Member Satisfaction Initiatives: Innovations benefit payers because they foster trust to ultimately drive the healthcare experience of members.
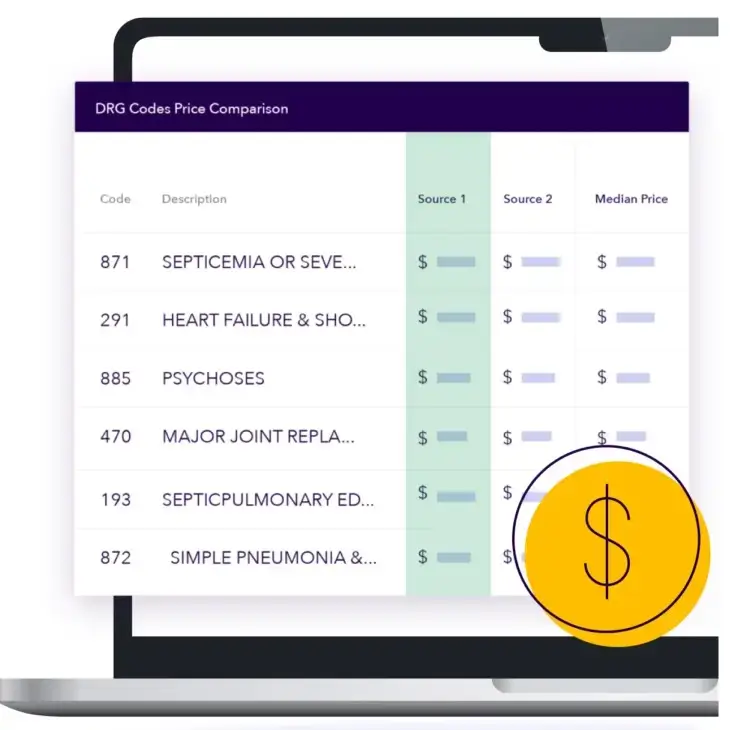
In-Network Pricing: Reducing Costs and Enhancing Value
How Zelis Helps Healthcare Providers and Members with In-Network Claims
Zelis also makes sure that things are on a fast track when it comes to processing in-network claims. This in turn helps cut costs and reduce misunderstandings in members and providers. Key benefits include:
- Accurate Pricing: Measures that help to achieve the ultimate goal of making sure that providers and members comprehend related costs in respect to in network care.
- Streamlined Communication: Efficiency grows out of the collaboration among the players with a positive impact on the time of decisions on claims.
- Cost Transparency: One advantage of the plan is that members are able to locate cheap, in-plan options quickly.
How Payers Control Costs for In-Network Claims
To payers, in-network pricing solutions can also assure that although cost is contained in a specific way, quality is not compromised. By leveraging Zelis’s tools, payers can:
- Negotiate Better Rates: The payers get benefits such as information on competitive pricing.
- Reduce Administrative Costs: They cut out human related mistakes and delay that may come as a result of repetitive tasks.
Member Engagement: Guiding Members Through the Healthcare Journey

How Zelis Helps Members Navigate Healthcare
Zelis empowers members with the knowledge that enables them to make right choice for their health management. These tools help members:
- Find Affordable Care: Providers can only treat patients if they are in their network and in different specialties at that.
- Stay Healthy: With the help of the given option, I will be able to participate in wellness programs and receive preventive care resources.
- Get Rewarded: Take advantage of incentives for selection of improving solutions and strategies with least costs.
How Zelis Supports Providers with Data Insights
Providers have an opportunity to enhance their member interaction thanks to the data Zelis offers. This includes:
- Improved Communication: Aids that can enhance effective patient relations.
- Actionable Insights: APM to manage and organize datasets That would help the practitioners and other stakeholders involved understand the patient needs and enhance patient care.
Out-of-Network Solutions: Managing Rising Costs
Out of network claims can be an issue for both providers, members and payers This challenge may be small for one of the players but it may be huge for the other. Instead, Zelis provides plans that help deal with these challenges.
The Rising Cost of Out-of-Network Claims
The out of network claims costs tend to be higher and are not very convenient to anticipate. Zelis addresses these issues by:
- Providing Reimbursement Solutions: They understood that it is important to have fair pricing strategies that will be suitable to blow all the stakeholders in the supply chain.
- Expert Negotiations: In making sure that providers and payers have arrived at what are reasonable prices for their numerous services.
Zelis’s Out-of-Network Tools
- Network Pricing Models: To serve as a tool in helping in cost controlling without reducing the quality of care being offered.
- State-Based Pricing: Ad-hoc solutions to suit the regions needs.
- Educational Resources: Blogs, podcasts, and webinars that guide stakeholders through complex scenarios.
Reference-Based Pricing for Network Replacement
Reference Based Pricing (RBP) is an innovative approach that has eliminated the costly convention of networks. There are key benefits with using Zelis’s RBP solutions.

What Is Reference-Based Pricing?
RBP sets the standard of prices for healthcare services so that the cost is reasonable and competitive. For this, it brings improvement in the sides of overpayment and an overall development of predictable and reasonable pricing models.
How RBP Helps Providers and Payers
- For Providers: RBP also removes billing complications and guarantees on time cash flow.
- For Payers: Organization costs are cut down to the minimal while offering top quality care through implementing RBP.
Payment Integrity: Ensuring Accuracy and Savings

How Zelis’s Payment Integrity Solutions Work
As compared with other similar health care technologies, Zelis minimizes error percentages but also cuts healthcare costs at the similar time. Key aspects include:
- Claims Editing: Other sub-programs which literally guarantee that a claim made is correct..
- Flexible Configurations: Particular particular activities that are peculiar to the requirements.
- Comprehensive Analytics: Policies and procedures for effectively determine loop holes in organizations and advise on how best those organizations could be run.
Maximizing Savings
In other words, there’s a lot that Zelis can do for everyone, especially when it comes to slashing the amount spent on costly billing errors.
Payments Optimization: Streamlining Healthcare Transactions

The Role of Zelis’s ZAPP Platform
ZAPP of Zelis brings innovation to the payment process in healthcare. Key features include:
- Streamlined Payments: Reducing transaction time is important because it saves time and increases on cash flow.
- Variety of Payment Options: Options tailored to individual needs.
- Consumer-Centric Design: The focus of stakeholders’ engagement is on ensuring that all of them receive positive impressions.
Partnership Network
This means that Zelis works with all its partners to spread the access throughout the market and make it easily solutioned.
How Zelis Supports Healthcare Providers

Faster Payments and Business Growth
Zelis helps providers improve cash flow and grow their businesses by:
- Connecting Providers with Payers: Employing a wide array of providers, and growing the number of patients and payers exposed to their programs.
- Reducing Administrative Costs: New systematic approaches make it possible to regain the time dedicated to patient treatment.
Solutions for Providers
Zelis offers tailored solutions for:
- Provider Networks: Improving communication between managed care organizations as providers and other payers.
- Electronic Payments: Ensuring timely reimbursements.
- Payment Integrity Services: Proper handling of the claims for the maximum achievement.
Read Also: How to Enroll in Zelis Payments?
Conclusion
Zelis comprehensive solution portfolio is relevant to the issues that affect healthcare most. Whether it is network management or payment accuracy, Zelis is assisting providers, its members and payers in attaining improved results at a lower cost. In so doing, Zelis is playing the role that creates the future of healthcare through collaboration and transparency.
FAQs
What is Zelis Network Solutions?
Zelis Network Solutions links providers, members, and payers to manage health delivery and enhance the member, system, and/or payer experience.
How does Zelis manage in-network claims?
Zelis thus employs elements that will help in giving accurate tariffs, minimize on the costs in administration, and bring out clarity for the in-network claims.
What is Reference-Based Pricing (RBP)?
RBP is a plan that sets standard prices of services that may be used in healthcare delivery to avoid exploitation.
How does Zelis optimize healthcare payments?
Zelis ZAPP facilitates payments, provides choice and improves cash flows.
What resources does Zelis provide for out-of-network claims?
Zelis has a full service reimbursement solutions in and out of network, along with its negotiation and educational tools that assist to minimize out of networks claim.